high heart rate after surgery
:max_bytes(150000):strip_icc()/can-i-have-surgery-if-i-have-high-blood-pressure-1764089_final-14bfea7fe13247ee95b3d53000c86fa9.jpg) High Blood Pressure Before, During, and After Surgery
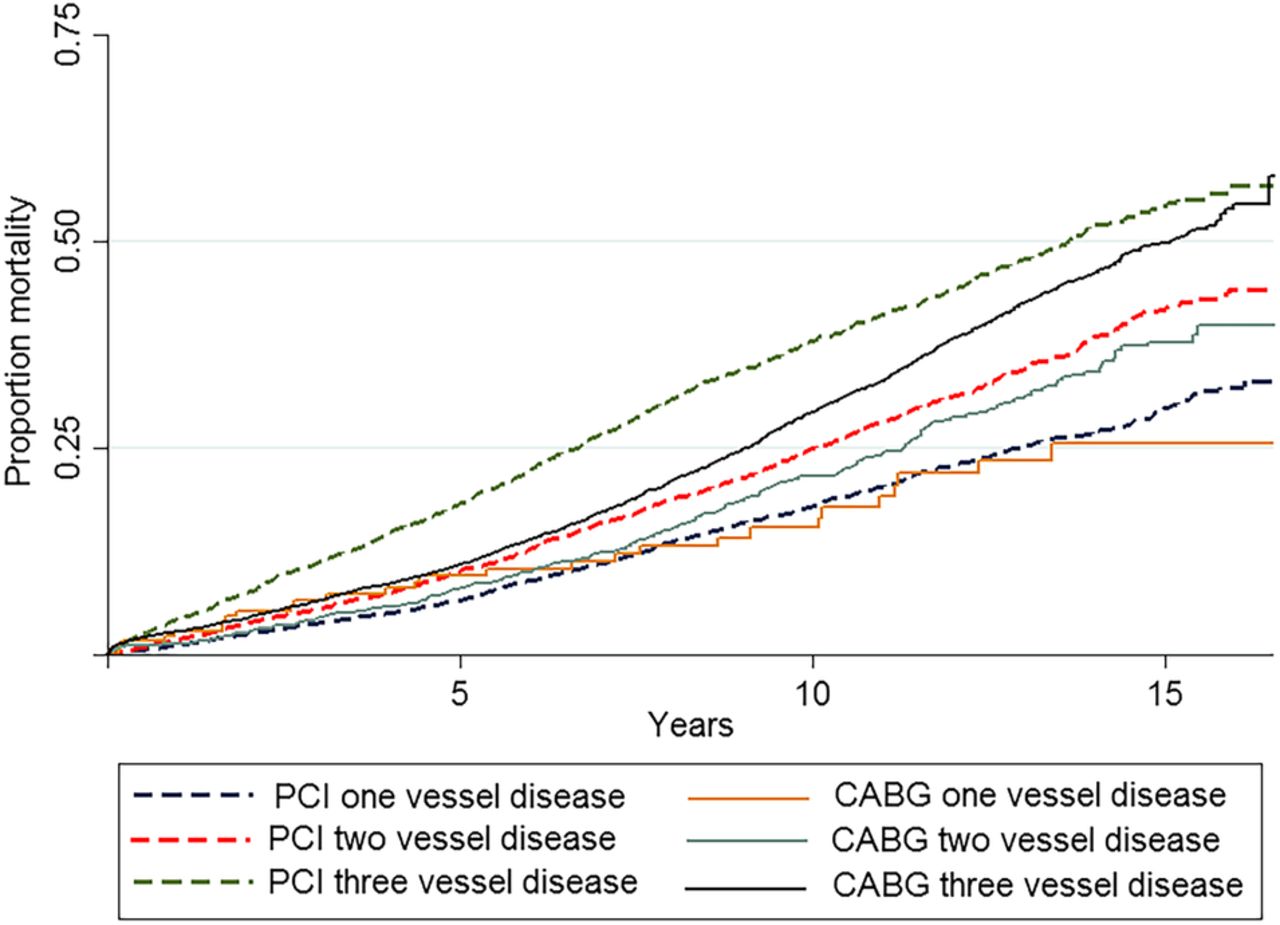
High Blood Pressure Before, During, and After SurgeryAnnouncement Effect of oxygen treatment on heart rate after abdominal surgery (Rosenberg-Adamsen) Registrar.(Lie, Bernhard) Student Doctor.(Kehlet) Professor of Surgery.(Rosenberg) Consultant. Susan Rosenberg-Adamsen, Claus Lie, Anne Bernhard, Henrik Kehlet, Jacob Rosenberg; Effect of Oxygen Treatment on Heart Rate After Abdominal Surgery . Anesthesiology 1999; 90:380-384 doi: Download dating file: Cardiovascular complications are common during the postoperative period and may be associated with hypoxemia and tachycardia. Preliminary studies in high-risk patients after surgery have shown a possible beneficial effect of oxygen therapy on oxygen arterial saturation and heart rate. The authors studied the effect of oxygen therapy in the arterial oxygen saturation and heart rate in 100 consecutive patients without random and double-blind choice assigned to receive air or oxygen therapy between the first and fourth day after the main abdominal surgery. The median rate of oxygen saturation increased significantly from 96% to 99% (P Postoperative oxygen therapy increased the arterial oxygen saturation and the decrease in heart rate after uncomplicated abdominal surgery in a consecutive group without the choice of patients who received routine postoperative care. This article is accompanied by an Editorial View. Please see: Weiskopf RB: Simple, easy, safe and cheap. But is it effective? Anesthesiology 1999; 90:358-9 MAJOR surgery may be followed by complications such as myocardial infarction, wound infection, wound healing and ventilation disorders. This cannot be explained only by imperfections in surgical techniques, but can be caused by greater demands of organs caused by endocrine metabolic response to surgical trauma. The most common complications are heart and represent more than half of the deaths occurring after surgery. Postoperative myocardial ischemia is an important predictor of adverse heart results after non-heart surgery, and research has suggested that prolonged subendocardial ischemia rather than acute coronary occlusion is the predominant mechanism of infarction after major surgery. Postoperative myocardial ischemia is often associated with tachycardia, and episodic tachycardia and episodic hypoxemia may occur concomitantly after the operation. In addition, postoperative episodic hypoxemia may be related to the occurrence of myocardial ischemia. Myocardial ischemia can result from a reduction in the supply of oxygen and increased demand. Thus, a simultaneous reduction in the delivery of myocardial oxygen and an increase in the consumption of heart oxygen as a result of the coexistence of arterial hypoxemia and tachycardia represent defavorable postoperative conditions for the heart. In a preliminary study in 12 patients after the surgery that had hypoxemia ( oxygen saturation [SpO2] 90 beats/min), oxygen therapy significantly increased SpO2 and reduced HR. It is not known, however, if oxygen supplementation will increase blood SpO2 and decrease HR in all patients after surgery. Therefore, we evaluate the effect of oxygen therapy on SpO2 and arterial HR in a large group of consecutive and unselected patients after major abdominal surgery. Materials and Methods Our local ethics committee approved the study, and patients gave written consent. One hundred patients were recruited for the study. All patients were subjected to major abdominal operations and received routine perioperative care. Patients who received pre- or postoperative oxygen therapy were not included in the pavilion or pharmacological treatment with [small beta, Greeks] blockers, calcium antagonists or digoxin. There were no restrictions on inclusion in relation to SpO2or HR. The study was performed as a test session in the surgical pavilion during the day between the days 1 and 4 and only the days of the week. The population of the study consisted of 51 men and 49 women, with a median of 60 years (range, 19-97 yr), a height of 171 cm (range, 150-190 cm), and a weight of 55 kg (range, 40-110 kg). Forty-eight patients were subjected to colorectal procedures, 23 were subjected to gastroduodenal procedures, 10 were subjected to exploratory laparotomy, 9 were subjected to small bowel resection, 8 were operated for adhesions, and 2 were subjected to open colectomy. Sixty-two patients received epidural anesthesia combined with enflurane, isoflurane, propofol or midazolam and low-dose fentanyl. Postoperative analgesia consisted of an epidural regimen of 4 ml/h of a mixture of bupivacaine (2.5 mg/ml) and morphine (50 [micro]g/ml sign), except in two patients, who received 2 ml/h of this epidural mixture. Postoperative epidural analgesia was complemented by 1 g paracetamol four times a day. Thirty-eight patients did not receive epidural anesthesia (acute surgery), and in these the main anesthetic agent was isoflurane (n = 25), midazolam and low-dose phentanile (n = 6), enflurane (n = 5), or propofol (n = 2). In these patients, postoperative analgesia consisted of 1 g paracetamol four times a day and intramuscular morphine of 5-10 mg or 10-20 mg orally on demand. The study had three parts that all used a catheter of delivery of kinase oxygen. In period 1 (control), patients received 3 l/min air for 30 min; in period 2, they received 3 l/min 100% oxygen for 30 min; and in period 3, they received 3 l/min air for 30 min. Each monitoring period was preceded by a period of 15 minutes in which patients became accustomed to inhalation using the Binasal oxygen catheter and receiving air or oxygen (similar to the next monitoring period). Periods 2 and 3 were reversed randomly. Oxygen saturation and RRH were measured continuously with pulse oxide (Nellcor N-200; Nellcor Puritan Bennett, Pleasanton, CA) and an adhesive finger probe. The data were displayed at 1-s intervals and entered into a bed computer with later printing and data analysis. The patient and the observer performing the data analysis were blinded to the order of the inhalation regime. For statistical analysis, we use Spearman's correlation test, linear regression analysis, Wilcoxon's range test, Mann-Whitney U test, and Kruskal-Wallis' corrected tie test. P The average duration of the surgery was 130 min (range, 35-300 min). The duration of the general anesthesia was 165 min (range, 55-370 min). In the first period (air), the median SpO2 was 96% (range, 84-100%) and the HR was 84 strokes/min (range, 56-160 beats/min). During oxygen supplementation, SpO2 increased to 99% (range, 94-100%; Figure P 1. (A) Heart rate and (B) oxygen blood saturation (SpO2) after oxygen or air supplementation by random order (mediums and quartiles)*P Figure 1. (A) The heart rate and (B) the blood saturation of oxygen (SpO2) after oxygen or air supplementation by random order (medium and quartile)*P (A and B) show the change of HR during oxygen therapy, Delta HR, in relation to the SpO2y HR prestudy-control. Comparing Delta RRHH for the initial defined subgroups of HR, we find a significant reduction in HRH with oxygen in patients with initial RRH of 110 strokes/min or more compared to patients with HRD of 70 strokes/min or less (P Figure 2. Changes in heart rate (Delta HR) after oxygen supplementation for defined subgroups of oxygen blood saturation (SpO2) with air (A) and heart rate (HR) with air (B) (median and quartile). The Kruskal-Wallis test produced P = 0.12 in A and P = 0.02 in B.Figure 2. Changes in heart rate (Delta HR) after oxygen supplementation for defined subgroups of oxygen blood saturation (SpO2) with air (A) and heart rate (HR) with air (B) (mediums and quartiles). The Kruskal-Wallis test produced P = 0.12 in A and P = 0.02 in B. Patients with low initial SpO2 values had a tendency towards a more pronounced reduction in HR with oxygen therapy, although this was not significant (P = 0.06 and P = 0.12;A). The results of the linear regression analysis (P = 0.18) and the correlation test (P = 0.37) between SpO2 and Delta HR were not significant. Thirty-five patients were studied on postoperative day 1, 32 on postoperative day 2, 19 on postoperative day 3 and 14 on postoperative day 4. No significant differences were found in HR with air or oxygen (P = 0.3 and P = .4), changes in HR (P = .5), SpO2 with air or oxygen (P = 0.06 and P = .5), or changes in SpO2(P = .052) among patients studied in the different postoperative days. Patients who received epidural analgesia had significantly lower HR values when receiving air (average 79 versus 90 beats/min, P 0.2) and did not significantly relate to Delta HR (linear return, P = .90; Spearman correlation, P = .78). Debate This study shows a reduction of HR with oxygen therapy during the late postoperative period, and was more pronounced in patients with high RRH or low SpO2 values. Therefore, oxygen therapy may have a positive effect on the supply of heart oxygen and the balance of consumption in patients not selected after the operation. These findings are of clinical importance, as several studies have found a relationship between postoperative myocardial ischemia and elevated HR. In addition, episodic tachycardia and episodic hypoxemia can occur concomitantly in the late postoperative period. Myocardial ischemia can result from a reduction in the supply of oxygen and increased demand. Late postoperative hypoxemia is commonly seen after major abdominal surgery, with a minimum in the second and third nights postoperative. Myocardial ischemia and infarction occur with a maximum incidence during operation and on the third postoperative day. Postoperative hypoxemia, which leads to decreased oxygen supply to body organs, was shown in previous studies that were temporarily associated with myocardial ischemia and therefore may be a factor contributing to the development of postoperative myocardial infarction. The findings of a study in which most postoperative myocardial infarctions were non-Q wave infarctions caused by long-term subendocardial ischemia rather than coronary occlusion support this hypothesis. The importance of postoperative tachycardia for myocardial ischemia has been described by Mangano et al. and other researchers, and Weiskopf et al. showed the association between the increase in HRH and the consumption of myocardial oxygen probably increased. The clinical relevance of our results is also supported by an interventionist study in 300 patients receiving Mivazerol, a new [small alpha, Greek]2-adrenoceptoragonist, which reduced the incidence of postoperative myocardial ischemia in relation to a reduction of HR that was comparable to the reduction we found in the current study (5-10 beats/min). In addition, a study of the effect of perioperative use of atenololol in 200 high-risk patients under non-cardiac surgery showed a reduction in the mortality rate and the incidence of cardiovascular complications for up to 2 years after surgery. The mechanism of reducing HR after oxygen supply is not fully understood. A reduction of HR after oxygen has been found in patients with chronic lung disease and liver cirrhosis and in non-surgical patients with chronic heart failure during a stress test by bicycle. In addition, in a study on healthy rest volunteers, a significant reduction of HHR was observed during oxygen breathing, with a decreased heart rate simultaneously and increased peripheral vascular resistance and blood pressure. In addition, in a recent study in conscious healthy patients and volunteers, a decrease in the blood oxygen content and a reduction in the delivery of oxygen in tissue resulting from an isovolemic reduction of blood hemoglobin caused a decrease in systemic vascular resistance and an increase in HR, the volume of strokes and the heart rate. Because of these results, a possible sequence of events after oxygen inhalation, and therefore the increase in blood oxygen content, may be the constriction of the peripheral vascular bed with an increase resulting from blood pressure and the subsequent slowing of HR due to the baroreceptor sinus carotid reflex. Another mechanism that triggers the reduction of HR with supplemental oxygen can be a reduction of the sympathetic tone, because Becker and Kreuzer showed that exposure to low oxygen pressure stimulating 3,000 to 4,000 m of altitude increased the excretion of epinefrine but not changed in healthy adults. This can be supported by findings of a decrease in the arterial concentration of epinefrine and a reduction of HR after oxygen was supplied to patients with cirrhosis. Thus, reducing sympathetic nerve activity can be a plausible explanation for the effect of oxygen supply on HR changes in patients after surgery. In the preliminary study in patients with concomitant hypoxemia (SpO2 90 beats/min), we find a significant reduction in HR (median 6 beats/min) after the supply of oxygen in each of the 12 patients studied. In the current study, we decided to deliberately include a large group of unselected patients; that is, we also tested patients without hypoxemia and tachycardia between the 1 and 4 days after the operation, although we know that hypoxemia is worse in postoperative days 2 and 3. We did so to potentially generalize the implications of our study depending on the results. We found that 73% of patients responded with decreased HR after oxygen was provided and that the most pronounced changes were observed in patients with pre-existing tachycardia and hypoxemia, although this was not statistically significant (A and B). When the current results are considered with those of our previous sample of patients who all had hypoxemia and tachycardia, it is obvious that the response to the decrease in HRD to oxygen treatment is more pronounced in patients with pre-existing tachycardia. This seems to support the assumption that the sympathetic reflection described in the postoperative oxygen supply would be more pronounced in high-risk patients. Although the study was not designed for an additional subanalsis of the results, we found significantly lower-based HRH in patients who received epidural analgesia compared to patients who received intramuscular morphine, probably due to reduced activity in the sympathetic nervous system. However, the HR response to oxygen supplementation was similar in patients with and without epidural analgesia. In addition, we find answers similar to oxygen administration in the different postoperative days studied, and no age effect in the response of HRH to oxygen therapy. As noted above, hypoxemia and tachycardia are potential risk factors for the development of postoperative myocardial ischemia. In addition, hypoxemia can be a factor that contributes to the development of postoperative complications, such as heart arrhythmias, healing of wounds with deficiencies and mental confusion. Our current results favor the administration of oxygen to patients after surgery and add more weight to the growing body of evidence of the benefits of postoperative oxygen therapy. It may be argued that an indication for postoperative oxygen therapy could be the presence of tachycardia regardless of the levels of blood oxygen. However, until controlled studies have shown that oxygen treatment decreases postoperative morbidity and mortality rates, final recommendations for the routine administration of postoperative oxygen should still be made. REFERENCES Cite articles through More seen More Cited Email alerts Related articles Social networks or
High Heart Rates After Heart Surgery: Patient Discussion
/anemia-after-surgery-3156852-Final-63c258f51d7846e1b24d870a3b8ea88c.png)
Postoperative Risks of Anemia and Blood Loss
High Heart Rates & Loud Heartbeats After Cardiac Surgery

High Heart Rates After Heart Surgery? Loud Heartbeats After Cardiac Operations? - YouTube

Changes in Heart Rate Variability after Coronary Artery Bypass Grafting and Clinical Importance of These Findings

High Blood Pressure After Surgery: 6 Possible Causes

What is Your Pulse and Heart Rate Trying to Tell You? | Health Plus
/temperature-after-surgery-3156832-02-5b5626b646e0fb00371d6a4f.png)
When Does Fever After Surgery Become a Concern?

Elevated preoperative heart rate is associated with cardiopulmonary and autonomic impairment in high-risk surgical patients - ScienceDirect

Can You Avoid Irregular Rhythm After Heart Surgery? – Health Essentials from Cleveland Clinic

What It Means If You Have Low Blood Pressure But a High Heart Rate – Health Essentials from Cleveland Clinic

How to lower your heart rate: 11 ways

Total heart rate variability (HRV) and low to high frequency ratio... | Download Scientific Diagram

Heart rate: What is a normal heart rate?
:max_bytes(150000):strip_icc()/sinus-bradycardia-1746253-01-912dc3d6234044d6a2fe921327efb28d.png)
Bradycardia: When is a Slow Heart Rate a Problem?

What is Your Pulse and Heart Rate Trying to Tell You? | Health Plus

Is your heart healthy enough for surgery? - Harvard Health

Tachycardia: Fast Heart Rate | American Heart Association
/what-is-a-quintuple-bypass-surgery-3157253-color012-21a01d9e23904490a252df8df9bff409.jpg)
What Is a Quintuple Bypass Surgery?
Elevated heart rate after non-cardiac surgery: post-hoc analysis of a prospective observational cohort study

How to lower your heart rate: 11 ways
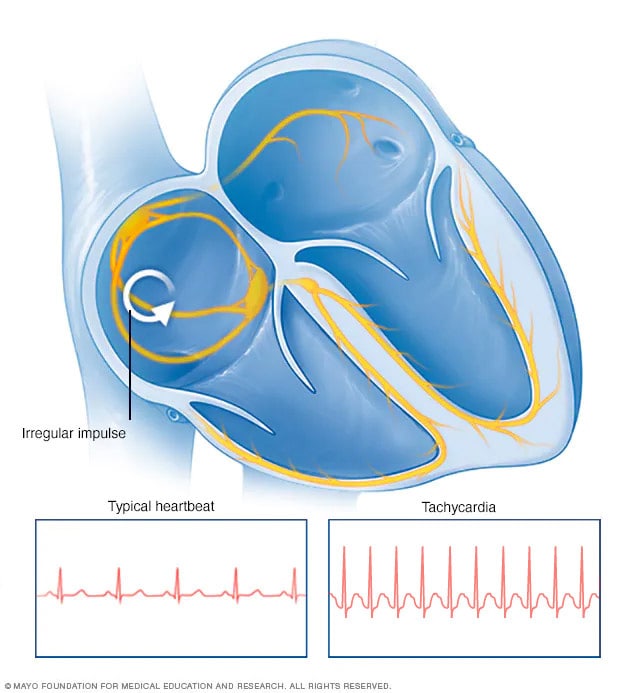
Tachycardia - Symptoms and causes - Mayo Clinic

What Causes Low Blood Pressure After Surgery?

Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study - The Lancet
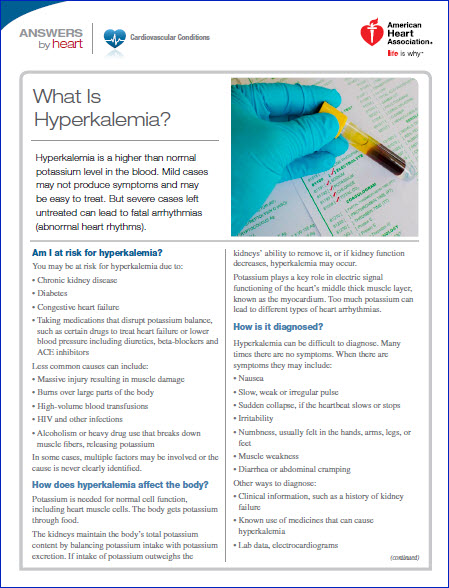
Hyperkalemia (High Potassium) | American Heart Association

How's your heart rate and why it matters? - Harvard Health

Tachycardia - Symptoms and causes - Mayo Clinic
High Heart Rate After Bypass Surgery - Rating Walls

A) Histogram of RR intervals on 24-hour Holter ECG: (A1) initial and... | Download Scientific Diagram
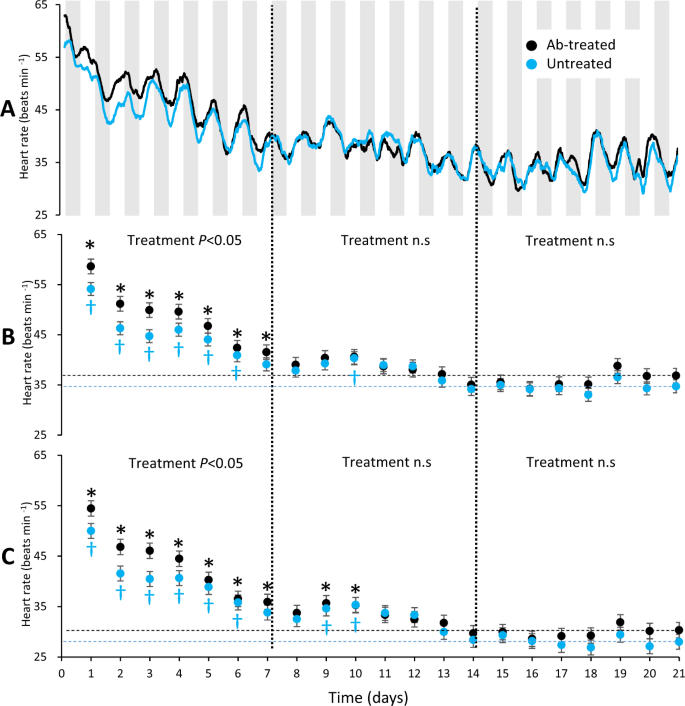
Effects of prophylactic antibiotic-treatment on post-surgical recovery following intraperitoneal bio-logger implantation in rainbow trout | Scientific Reports
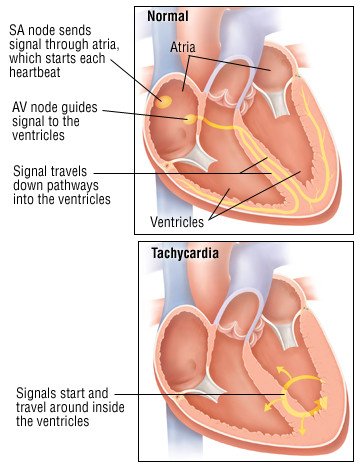
Tachycardia Guide: Causes, Symptoms and Treatment Options

Fast heart rate (tachycardia)

Heart Rate Recovery: Powerful Prognosticator Now on Apple Watch | MedPage Today

How to Keep Your Heart Healthy After Surgery | Everyday Health

Low Heart Rate – Bradycardia Explained by a Heart Doctor • MyHeart
Atrial fibrillation: Common, serious, treatable - Harvard Health

Heart bypass surgery: Procedure, recovery time, and risks

What Causes Low Blood Pressure After Surgery?

The obesity paradox: Obese patients fare better than others after heart surgery

Can cervical spine instability cause heart palpitations and blood pressure problems? – Caring Medical Florida
Posting Komentar untuk "high heart rate after surgery"